Health
Ovestin: Understanding Its Uses, Benefits, and Evolving Scientific Insights
Ovestin, a medication containing the naturally occurring estrogen estriol, has become an important therapeutic option for women experiencing symptoms related to estrogen deficiency. Commonly prescribed during peri-menopause, post-menopause, and after certain gynecological procedures, stands out from other estrogen therapies due to its mild potency, localized action, and favorable safety profile. As medical understanding continues to evolve, renewed attention has been given to estriol’s unique interaction with estrogen receptors and its potential role in protecting vaginal and urinary tract health. This article explores the foundational science behind Ovestin, its primary uses, emerging insights, safety considerations, and the ways clinicians are refining treatment approaches for women.
What Is Ovestin and How Does It Work?
Ovestin is formulated with estriol, one of the three main estrogens in the female body. Unlike estradiol and estrone—both significantly stronger—estriol acts as a short-acting, weaker estrogen that primarily binds to estrogen receptor-beta sites. These receptors are heavily concentrated in tissues of the vagina, vulva, cervix, urethra, and bladder, explaining why effects are especially prominent in these areas.
When applied vaginally or taken orally (depending on the formulation), Ovestin helps restore thinning mucosal tissues, increases blood flow, improves lubrication, and enhances epithelial resilience. Because estriol is rapidly metabolized and poorly retained systemically, its effects remain largely localized, making it a valuable option for targeted therapy.
Ovestin for Menopause-Related Vaginal Symptoms
One of the most established uses for Ovestin is the treatment of vaginal atrophy, also known as genitourinary syndrome of menopause (GSM). Symptoms such as dryness, irritation, burning, and discomfort during intercourse arise primarily from declining estrogen levels. Ovestin’s ability to thicken vaginal tissues and restore natural lubrication has made it a first-line treatment for many clinicians.
Unlike systemic hormone replacement therapy (HRT), which affects the entire body, Ovestin can be administered locally via vaginal cream or suppositories. This allows women to experience significant symptom relief with minimal systemic hormone exposure. Many women begin noticing improved comfort within weeks, and with ongoing use, the benefits often become more sustained.
Supporting Urinary and Pelvic Health
A growing area of medical interest involves Ovestin’s impact on urinary and pelvic health. Because estrogen receptors are also found in the urethra and bladder, declining estrogen in menopause often contributes to increased frequency, urgency, mild urinary leakage, and recurrent urinary tract infections (UTIs). Restoring localized estrogen levels can help strengthen pelvic tissues, improve urethral closure pressure, and reduce vulnerability to infections.
Recent clinical discussions suggest that estriol’s unique receptor activity may play a role in enhancing the natural protective microbiome of the vagina and urinary tract. This aligns with emerging evidence showing that estriol helps restore populations of lactobacilli—beneficial bacteria that create an acidic environment hostile to harmful microbes. Although research is ongoing, many clinicians already incorporate Ovestin into prevention strategies for recurrent UTIs in post-menopausal women.
Ovestin vs. Stronger Estrogen Therapies
One key advantage of Ovestin is its lower systemic impact. Estriol’s weak estrogenic activity reduces the likelihood of systemic side effects compared to stronger estrogens like estradiol. This has led to increased use of Ovestin in women who cannot tolerate or prefer to avoid systemic HRT.
Because estriol does not stimulate the uterus or breast tissue to the same degree as stronger estrogens, Ovestin is often considered suitable for women seeking localized relief without whole-body hormone exposure. However, it is important to emphasize that all forms of hormone treatment should be supervised by a healthcare professional, particularly for women with a personal history of hormone-sensitive conditions.
Formulations and Methods of Use
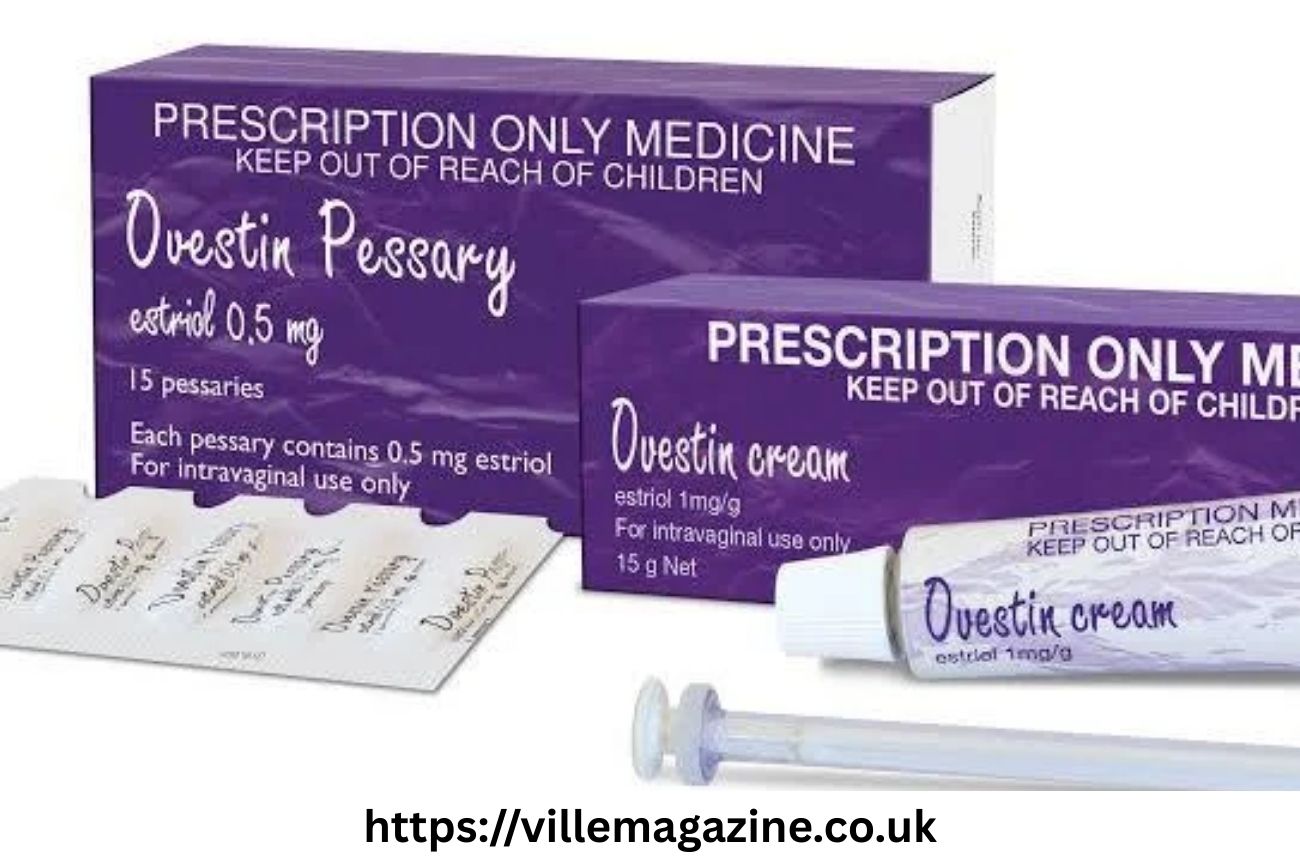
Ovestin is available in several formats, most commonly as:
-
Vaginal cream: Applied using an applicator for even distribution
-
Vaginal pessaries/suppositories: Convenient for internal release
-
Oral tablets: Less common and used more selectively
The vaginal route is preferred for targeted therapy, as it maximizes local efficacy and minimizes systemic absorption. Treatment typically begins with a more intensive daily schedule for several weeks, followed by a reduced maintenance dose. Physicians personalize dosing to ensure both effectiveness and minimal exposure.
Benefits for Sexual Well-Being
Beyond physical symptoms, vaginal atrophy can influence intimacy and overall well-being. Painful intercourse, reduced lubrication, and irritation can create anxiety surrounding sexual activity. Ovestin helps restore comfort, elasticity, and moisture, which can significantly improve sexual function and confidence.
Additionally, because estriol increases blood flow to the vaginal region and supports tissue regeneration, many women report improved sensitivity and comfort over time. These improvements contribute not only to physical health but also to the emotional and relational aspects of sexual well-being.
Safety Profile and Clinical Considerations
Ovestin is generally well-tolerated, with the most common side effects being mild local irritation or transient spotting during the first weeks of therapy. These effects usually diminish as tissues heal. Since systemic absorption is minimal, the risk of systemic estrogenic side effects is much lower than with other forms of HRT.
Still, healthcare providers evaluate medical history carefully, especially for individuals with:
-
Breast cancer history
-
Endometrial conditions
-
Unexplained vaginal bleeding
-
History of blood clots
Though estriol’s risk profile is comparatively favorable, medical guidance ensures safe and appropriate use.
Evolving Insights into Estriol and Immune Modulation
An area of expanding scientific interest involves estriol’s potential role in immune modulation. Researchers have studied estriol’s influence on inflammatory pathways, suggesting that its receptor interactions may help regulate tissue healing, immune resilience, and mucosal protection. While these findings are in early stages, they have encouraged renewed attention to estriol’s multifaceted biological role, particularly in menopausal health.
Although not yet part of official treatment guidelines, these scientific discussions highlight estriol’s potential reach beyond surface-level symptom relief. Continued study may clarify how localized estriol therapy supports the broader health of vaginal and urinary tissues.
Impact on Vaginal Microbiome Restoration
Another emerging area of interest is Ovestin’s influence on the vaginal microbiome. Estrogen deficiency often leads to a reduction in lactobacilli and an increase in vaginal pH, creating an environment more susceptible to infections and irritation. Clinicians have observed that Ovestin helps reverse these changes by restoring tissue health and encouraging the return of protective bacterial populations.
This microbiome-restoration effect contributes to long-term genital health and has become an increasingly recognized reason for prescribing Ovestin—especially for women experiencing recurrent irritation or post-menopausal infections.
Integrating Ovestin into Broader Menopause Care
Ovestin is frequently used as part of a comprehensive menopause care plan. Alongside lifestyle strategies such as pelvic-floor exercises, hydration, and sexual health counseling, Ovestin provides targeted relief that complements broader wellness approaches. Many women use Ovestin long-term as a maintenance therapy to preserve vaginal and urinary health.
Clinicians may also combine Ovestin with systemic HRT when addressing whole-body menopausal symptoms while still prioritizing localized treatment for vaginal concerns.
Clinical Perspectives and Future Directions
As research advances, medical professionals continue to refine the therapeutic role of estriol-based treatments. The ongoing exploration of estriol’s receptor selectivity, microbiome effects, and immune interactions suggests that Ovestin may have broader implications than previously recognized. While more formal studies are needed to solidify these insights, early observations support the medication’s value in promoting tissue regeneration, comfort, and genitourinary stability.
The safety profile and localized action of Ovestin also position it well for future inclusion in advanced treatment protocols, particularly for women seeking hormone therapies with minimized systemic influence.
Conclusion
Ovestin remains a trusted, effective, and well-tolerated treatment for women navigating the challenges of estrogen deficiency, particularly those affecting vaginal and urinary health. By restoring tissue moisture, elasticity, and microbiome balance, Ovestin plays a crucial role in improving comfort, sexual well-being, and overall quality of life. As scientific understanding deepens, emerging insights into estriol’s unique biological interactions highlight even greater potential for this gentle yet powerful therapy. With proper medical guidance, Ovestin offers a reliable path toward renewed health and confidence for women at every stage of menopause.
-

 Celebrity9 months ago
Celebrity9 months agoNick Schmit? The Man Behind Jonathan Capehart Success
-
 Celebrity9 months ago
Celebrity9 months agoChristina Erika Carandini Lee: A Life of Grace, Heritage, and Privacy
-

 Celebrity9 months ago
Celebrity9 months agoTrey Kulley Majors: The Untold Story of Lee Majors’ Son
-

 Celebrity9 months ago
Celebrity9 months agoJamie White-Welling: Bio, Career, and Hollywood Connection Life with Tom Welling
















